
However, the patient immediately developed extensive subcutaneous emphysema with crepitus and hyper-resonant percussion on the left abdomen. Mechanical ventilator was recommenced without any sign of airway resistance. No active bleeding was noted after clot removal. The clots in the bronchi were removed and thrombin and epinephrine were given to control the bleeding ( Fig. Blood clots obstructed the airway from the distal trachea to both main bronchi. Fiberoptic bronchoscopy was performed to clear the airway and locate the source of bleeding.
Barotrauma lungs manual#
Manual ventilation was difficult, requiring considerable effort, because the trachea was partially obstructed by blood clots. Airway patency and saturation could be maintained only by manual ventilation using a self-inflated resuscitator bag. The SpO 2 was 74% and the patient was cyanotic. After 30 min, the ventilator “high airway pressure” and “low expiratory tidal volume” alarms sounded. Tranexamic acid was injected intravenously and packed red cells were transfused, followed by administration of tranexamic acid and epinephrine through the ETT to seek to control the hemoptysis. Mechanical ventilation was applied in pressure-controlled mode with a peak pressure of 26 cm H 2O, a positive end-expiratory pressure (PEEP) of 6 cm H 2O, a respiratory rate of 16 breaths/min, and an inspired oxygen fraction (FiO 2) of 1.0. Suction was applied to prevent asphyxiation about 300 mL blood was removed. Intubation was performed immediately but bleeding through the endotracheal tube (ETT) continued to be significant.

An initial chest X-ray revealed atelectasis in the left lung field ( Fig. Her white blood cell count was 3,460/mL, the hemoglobin level was 7.3 mg/dL, and the platelet count was 13,000/mm 3. Initial arterial blood gas analysis revealed a pH of 7.277, a pCO 2 of 49.9 mmHg, a pO 2 of 47.8 mmHg, and an SpO 2 of 76.6%. On admission, her initial vital signs were: blood pressure 150/100 mmHg, heart rate 152 beats/min, respiratory rate 34 beats/min, body temperature 36.6✬, and an oxygen saturation level of 60% in room air. She subsequently suffered severe graft failure and refractory pancytopenia. She had been diagnosed with aplastic anemia at 12 years of age and had received a bone marrow transplant 5 months prior. Case Report A 36 year old female was admitted with a 5-day history of hemoptysis and dyspnea. Here, we report a case of extensive subcutaneous emphysema, pneumothorax, and pneumomediastinum following manual ventilation of a patient who had an airway obstruction caused by massive hemoptysis. Airway occlusion by blood clots is fatal in cases of massive hemoptysis and is a significant risk factor for increased airway pressure in mechanically ventilated patients. The risk of excessive airway pressure is even greater during manual ventilation of an intubated patient, because air leakage is not possible. A high airway pressure is an important feature of the pathophysiology of barotrauma.
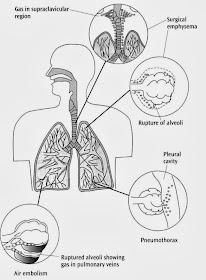
Keywords: airway obstruction barotrauma hemoptysis ventilationīarotrauma is a potentially lethal complication of positive-pressure ventilation.Nevertheless, the patient developed extensive subcutaneous emphysema, pneumothorax, and pneumomediastinum. Manual ventilation was initiated to improve oxygenation, and emergency flexible bronchoscopy was performed to clear the airway. However, airway obstruction by blood clots triggered desaturation and ventilator malfunction. A 36-year-old female patient with aplastic anemia developed massive hemoptysis and was placed on ventilator support.


 0 kommentar(er)
0 kommentar(er)
